Dog Health
Here are some examples of our research and the impact it has on companion animal health
How Dogs Could Help Doctors Find the Next Cure for Cancer
Dogs 10 years and older have a 50% chance of dying from cancer. They also develop the same types of cancers that humans do because their immune system is closely related to ours. Now human oncologists are studying cancer in canines in the hopes of benefiting both animals and humans. In this episode of Unfold, you’ll learn how UC Davis veterinarians and physicians are collaborating to help human cancer patients and their furry best friends.
In this episode:
Robert Canter, surgical oncologist with UC Davis Comprehensive Cancer Center
Michael Kent, radiation oncologist and director of the UC Davis Center for Companion Animal Health, School of Veterinary Medicine
Danae Unti, owner of Boone, a dog who completed a cancer clinical trial

UC Davis Osteosarcoma Clinical Trial Showing Success
Fred, a 6-year-old male shepherd cross, was diagnosed by his referring veterinarian with cancer in his left forelimb in April 2016. Due to preexisting orthopedic issues, he was not a candidate for the traditional amputation and chemotherapy treatment. Faced with only being offered palliative care for Fred, his dedicated owners, Rob and Linda, continued to hope and sought out other options. They discovered a new clinical trial at the UC Davis veterinary hospital that offered a cutting-edge approach to treating dogs with osteosarcoma.
“From the first meeting, we knew Dr. Michael Kent, Teri Guerrero (oncology clinical trials coordinator), and the entire UC Davis team would take great care of Fred,” Rob said.
The trial, sponsored by the National Cancer Institute (NCI) and being run in conjunction with the UC Davis School of Medicine’s NCI-designated Comprehensive Cancer Center due to a special interest in its future applications to human medicine, investigates the potential of a dog’s immune system to be manipulated to fight off its own cancer. After irradiating the tumor, veterinarians collect a particular type of the dog’s white blood cells, known as Natural Killer (NK) cells, then stimulate and grow the cells in a laboratory before injecting them back into the dog’s tumor. Ideally, the lung metastasis, or the spread of the tumor to the dog’s lungs (which occurs in more than 90 percent of osteosarcoma cases), will be slowed or stopped entirely by these NK cells.
Fred’s treatment started with palliative radiation to help control the local disease and reduce pain as well as to create a signal to the immune system that the NK cells could react to. He also began receiving monthly injections of zoledronate, a drug used to help prevent fractures in bones stricken with cancer. The following three weeks of radiotherapy ran seamlessly, and Fred’s sweet demeanor and fuzzy, lovable appearance quickly made him popular amongst the team of veterinarians, technicians, and students in the Oncology Service who cared for him.
Following radiation therapy, Fred received the first of two intratumoral NK cell injections without any complications. During the appointment for his second NK cell injection, Dr. Kent, the lead investigator on the trial, noticed Fred’s hesitation to bear weight on his left front leg. He consulted with the Orthopedic Surgery Service, and with the help of the Diagnostic Imaging Service, the team of veterinarians discovered fractures to both the radius (where the tumor was located) and the ulna, which is typical given the nature of Fred’s disease. A temporary splint was put in place and the second NK cell injection was given as planned. Several days later, orthopedist Dr. Po-Yen Chou surgically repaired Fred’s fractures.
By August, a CT scan revealed exciting news for both Fred and the osteosarcoma trial – there was no evidence of tumor spread or metastasis. Fred continued to receive zoledronate injections for two more months, and concluded his participation in the clinical trial at the end of October. His owners are thankful for the extension to Fred’s life that this trial has provided.
“No matter the long-term outcome, we feel he has received the very best of care, and that’s why we will always be grateful that UC Davis is able to offer clinical trials,” Linda said. “Making decisions in the treatment for pets that have cancer is never easy, but we have absolutely no regrets, and, as pet parents, that’s as good as it gets.”
This trial will have wide-reaching applications in both veterinary and human medicine. Over the last few years, immunotherapy has become the fourth arm in treating cancer, along with more traditional treatments such as surgery, radiation therapy and chemotherapy. By learning how to overcome immune tolerance and immunosuppression caused by the tumor, this study and other research UC Davis is conducting on immunotherapy hopes to provide oncologists more options for treating cancer in both pets and their owners.
Enamel hypoplasia in Samoyed dogs
 Samoyed dogs (as well as Italian Greyhounds and Standard Poodles) are affected by an inherited disease of enamel formation known as familial enamel hypoplasia (Amelogensis imperfecta).
Samoyed dogs (as well as Italian Greyhounds and Standard Poodles) are affected by an inherited disease of enamel formation known as familial enamel hypoplasia (Amelogensis imperfecta).
We are currently involved in research which we hope will lead to identification of the gene that is affected and the mode of inheritance. Potentially we may be able to develop a genetic test which could be used by breeders to to help them eliminate this disease from the breed.
For more information about this research and to learn how you can participate by sending samples and completing a survey, please see the links below:
Enamel hypoplasia research at CCAH (pdf)
Enamel hypoplasia - Survey Form (doc)
 Genetic Testing for Weimaraner Breeders Webinar Recording
Genetic Testing for Weimaraner Breeders Webinar Recording
This webinar was presented by Dr. Noa Safra in July 2014 and is directed to Weimaraner breeders and lovers. It provides information to allow breeders to use DNA tests available for the breed, in their breeding programs.
Topics addressed include testing for hyperuricosuria (HUU) and hypomyelination (shakey puppy). Also introduced is the concept of phenotypic testing for inherited disorders for which DNA tests are unavailable.
 Poodle Club of America Foundation supports study in sebaceous adenitis in Standard Poodles
Poodle Club of America Foundation supports study in sebaceous adenitis in Standard Poodles
The Poodle Club of America Foundation has provided funding to support a research project under the direction of principal investigator Niels C. Pedersen, "Determining whether risk for sebaceous adenitis of Standard Poodles is associated with a specific DLA class II genotype."
For additional information about this study please click on the appropriate link below:
Research Proposal: Sebaceous adenitis of Standard Poodles (pdf)
Manuscript: Genetic Characterization of Standard Poodles (pdf)
A Genetic Comparison of Standard and Miniature Poodles (pdf)
Information form for Sebaceous Adenitis study, to be submitted by dog owners and breeders (includes instructions regarding sample collection and submission) (pdf)
This project depends upon our ability to obtain DNA-containing specimens from at least 25 dogs with a confirmed diagnosis of sebaceous adenitis, in addition to specimens from unaffected dogs, preferably healthy close relatives. If you are a dog owner or breeder and are interested in participating in this study, please carefully read the information found at the above links.
- TOP -
Italian Greyhound Autoimmune Study
Researchers at the CCAH are currently undertaking research into a variety of canine autoimmune diseases, including autoimmune disease in Italian greyhounds.
 Additional information about the CCAH autoimmune study can be found on the "Italian Greyhound Genetic Diseases" survey form, which you can open in either.pdf format or MS Word document format (see below).
Additional information about the CCAH autoimmune study can be found on the "Italian Greyhound Genetic Diseases" survey form, which you can open in either.pdf format or MS Word document format (see below).
The form also includes instructions for submitting DNA samples. Italian Greyhound Genetic Diseases Survey Form (.docx)
Italian Greyhound Genetic Diseases Survey Form (.pdf)
- TOP -
Cutting-edge procedure helps pets with jawbone defects
The second phase in a clinical project with potentially major implications for both pets and people suffering from jawbone defects due to tumors, infections or injuries is now underway at the UC Davis School of Veterinary Medicine.
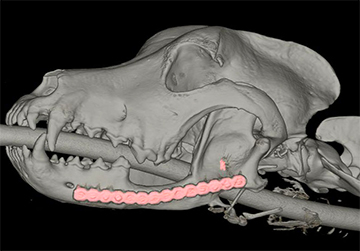
The mandible is a critical bone in the structure of the face. It is the largest, strongest and lowest bone in the face, and is responsible for forming the lower jaw and holding the lower teeth in place. But disease or trauma from injuries can cause problems with the mandible; particularly large defects that can’t be closed, like a significant fracture. Affected dogs suffer an enormous amount of difficulty eating. A dog might have to be fed only slushy foods, or through a stomach tube. Repairing the problem would allow the jaw to once again function normally.
Whiskey, for example, was a 9-year-old Munsterlander dog that could no longer chew food because of a cancerous growth on his jawbone. Veterinarians at our veterinary hospital performed a cutting-edge technique to help regrow the bone. Whiskey lived for four years after the procedure with an excellent quality of life.
That was back in 2012. Now, the focus is on using imaging to help doctors understand the procedure’s long-term safety, and whether this method can be used elsewhere in an animal’s body or eventually in humans. Dr. Rachel Pollard, an associate professor and researcher in the school’s Department of Surgical and Radiological Sciences, received a grant from the CCAH to research the computed tomographic (CT) assessment of bone and blood vessel regeneration following mandibular reconstruction with bone morphogenetic protein in dogs. Pollard is collaborating with doctors Boaz Arzi and Frank Verstraete, of the veterinary hospital’s Dentistry and Oral Surgery Service. "Nobody has done anything like this with either the bone regeneration or the imaging," Pollard says. “Both are totally new to veterinary and human medicine."
The mandibular regeneration procedure involves screwing a titanium plate into place to capture the natural contour of the jaw. The plate is unscrewed and the portion of the bone with the defect is surgically removed. The plate is screwed back onto the remaining bone, and a scaffolding material infused with “bone morphogenetic protein” is inserted into the gap to stimulate growth. Solid tissue begins to form after a couple weeks, and the scaffold grows bone cells.
Next, CT imaging is used to evaluate the bone regeneration over time — it assesses density, how well the defect has bridged and the impact on regional blood vessel development. Dogs in the clinical trial receive imaging prior to surgery, immediately afterward and at one, three and six months post-surgery. The research team has so far recruited three out of four cases. Once this current phase is complete, perhaps the cutting-edge technique to regrow the jawbone can one day translate to human medicine, as well.
"Overall, the mandibular reconstruction program at UC Davis has been running for more than three years and has revolutionized the way we treat mandibular bone defects," says Dr. Arzi. “We no longer have difficulties in regenerating bone across mandibular bone defects and, in most circumstances, dogs do not suffer from unstable jaw following cancer removal of non-healing jaw fractures."
- TOP -

Clinical trial aims to help ‘stuffy-nosed’ dogs
They’re nicknamed stuffy-nosed breeds for a reason. Bulldogs, Boston terriers, pugs, boxers, shih tzus, Pekingese all tend to have physical characteristics that lend themselves to breathing difficulties, including short noses and flat faces, narrowed nostrils and small windpipes.
Now veterinarians and researchers at the school are examining the response of brachycephalic dogs to upper-airway surgery, as part of a clinical trial currently underway. Specifically: How does this surgery impact the hiatal hernia, which refers to an organ — usually the stomach — protruding through the diaphragm’s esophageal opening?
“These dogs often have a combination of upper-airway obstruction, which makes it hard to breathe, and a hiatal herniation, which causes reflux disease,” says Dr. Philipp Mayhew. “The commonly held belief is that if you perform surgery to alleviate the upper-airway obstruction the signs associated with the hiatal hernia will resolve by themselves. But that’s not a theory that has ever been scientifically proven in an evidence-based manner. So we are testing that theory.”
This multi-departmental trial was spearheaded by Dr. Stanley Marks, professor in Medicine and Epidemiology, and Mayhew, associate professor in Surgical and Radiological Sciences. The trial has enrolled six cases so far, and will recruit cases for another one to two years.
Veterinarians conduct upper-airway surgery to repair the problem and with the owner’s permission follow up with a variety of diagnostic tests to analyze the effect on hiatal hernias. Among the tools being used is a high-resolution manometry (HRM) catheter to get a pressure profile of the esophagus from the upper esophageal sphincter, all the way down to the lower esophageal sphincter where the hernia occurs. The CCAH funded the purchase of this catheter. Marks and Mayhew agree the HRM catheter is a vast improvement over other diagnostic tools to evaluate the functions of the esophagus.
The next step in the trial involves asking owners for periodic updates and checking the esophagus for ulcers or erosions caused by stomach acid entering the area.
- TOP -

Study finds flawed claims on pet food labels
Choosing the right food for your pet can be a confusing process, but most of us take it for granted that the information found on pet food labels is always 100 percent correct and accurate. Not so, says Dr. Jennifer Larsen, an associate professor of clinical nutrition with the Nutrition Support Service.
Larsen co-authored a study, funded by the CCAH, investigating whether vegetarian diets — for both cats and dogs — marketed as “complete and balanced” were providing the levels of amino acids they claimed to contain, and whether these foods were accurately labeled. As it happened, many of them weren’t, on both fronts.
Of the 24 vegetarian diets the researchers studied, six did not contain adequate levels of one or more amino acids — organic compounds that play a critical biological function, helping to manufacture proteins within the body. “Some of the diets that were below the minimum weren’t just a little bit below,” Larsen says. “Some were as much as 34 percent lower than what was supposed to be there.” Amino acid deficiency is associated with several animal diseases, including skin diseases and dilated cardiomyopathy, a devastating heart condition.
Vegetarian diets are not the norm for most pets. However, some owners prefer to feed plant-based diets to their animals for ethical reasons, while other pets require non-meat diets due to specific health problems, including bladders stones, some types of liver disease and food allergies. But these diets can be difficult to balance. “When you formulate a diet for a dog or a cat using vegetarian protein sources, you have to be really careful that you’re doing it appropriately,” Larsen says.
The study, which was led by clinical nutrition resident Dr. Kayo Kanakubo with support from Larsen, also looked at the labels on these diets, and what they found there was more surprising. While the rules about pet food labeling can be confusing, most manufacturers follow the regulations set forth by the Association of American Feed Control Officials (AAFCO), which require them to disclose nine different categories of information on their labels, including calorie content and an ingredient list.
Only three of the 24 vegetarian diets the researchers studied had accurate labels that included all nine components. For example, seven diets got the guaranteed analysis wrong, seven had errors in their ingredient list and many didn’t have feeding directions. “If a company does not have accurate or legal labels, then I don’t have a lot of confidence that they can handle the many other details required to make a really healthful, wholesome and safe pet food,” Larsen says.
Larsen’s advice to pet owners: Be sure to read the nutritional adequacy statement on the label, which is often in tiny type on the back. This statement explains which species and life stage the diet is intended; whether the diet has a complete and balanced claim; and how the company substantiated that claim.
- TOP -

Nasal disease rampant among dogs and cats
Not too many clinician scientists want to study nasal disease in cats and dogs, a common syndrome that involves chronic mucus discharge from the nose and sneezing. It’s just too frustrating, explains Dr. Lynelle Johnson, a professor in the Department of Medicine and Epidemiology. Tests for nasal disease can be expensive and invasive — including MRI or CT scans, biopsies or rhinoscopy — and the results often difficult to interpret. Accordingly, this disease remains somewhat mysterious and its causes hard to pinpoint.
But Johnson is on the case because nasal disease is rampant. She wants to come up with the answers that could help so many cats and dogs, as well as their owners. “You can imagine a large-breed dog, like a German Shepherd, a collie or a Labrador retriever with nasal discharge all over the house. It’s a significant issue,” she says. “And cats, although they’re small, are equally problematic because they sneeze with such force that there’s discharge everywhere. Cats are particularly challenging because they will get worse, then better, then worse again, which also makes this disease so difficult to fully understand.”
Since joining the faculty in 2000, Johnson has devoted much of her research to both feline and canine nasal disease. She and her colleagues take a step-by-step approach to determining possible causes behind the disease. Her research is often made possible through grants generated by private donations to the CCAH.
Previous studies have examined a fungal infection in the nose of dogs, called Aspergillus. This fungal infection can destroy the nasal turbinates and other structures in the nose and lead to pain, sneezing and bleeding. Left untreated it can invade into the brain and be fatal. The researchers studied a blood test to diagnosis Aspergillus, and proved that if the result came up positive, the animal had the disease; although a negative result didn’t rule it out. That’s important because treatment for this fungal infection requires many hours under anesthesia. If the disease can be diagnosed early with a blood test, then veterinarians and owners can better prepare for the steps needed to treat the disease. Other studies have shown that the clinical signs of sneezing and nasal discharge don’t correlate with whether or not the dog has been cleared of fungus. People may think since the nasal discharge is gone, their dog must be cured. But that’s not true, which reinforces why accurate diagnostic tests and follow-up are so critical.
Nasal disease in cats has also been a focus of research. “It’s so common in the cat population, and although it’s often not life-threatening depending on the cause, it’s often about quality of life for the cat, as well as the human companion,” Johnson says. “Owners and veterinarians get very, very frustrated because you try all these different therapies but when you don’t know what causes a disease, you don’t know how to cure it.” The UC Davis team continues to investigate many infectious causes for feline nasal disease, while also evaluating management strategies for chronic nasal discharge.
- TOP -
New diagnostic procedure could assist dogs with large bowel disease
Dogs suffering from disease of the large bowel — the colon and rectum — may have diarrhea, severe constipation and bloody stool. These dogs are also generally older. Simply put, this disease is a dreadful condition as experienced by both the pet and its human companion. But developing a novel diagnostic procedure could improve a veterinarian’s ability to diagnose large bowel disease in a minimally invasive way, and allow for better surgical planning.
Veterinary researchers are currently studying the use of CT pneumocolonography for dogs with large bowel disease. This computerized tomography technique works by inflating the colon with gas, and then creating detailed scans that allow radiologists to clearly see this body part’s interior walls. The procedure could allow veterinarians to more precisely locate mass lesions and determine the extent of the disease.
Dr. Michele Steffey, an associate professor in the school’s Department of Surgical and Radiological Sciences, is the principal investigator on this project. “Masses of the large bowel are uncomfortable for patients and are best treated with surgical removal,” Steffey says. “But surgery can be challenging in this area, and the more information we can obtain preoperatively to plan the procedure, the better our outcomes are likely to be.” Faculty co-investigators include Dr. Allison Zwingenberger, Dr. Stanley Marks and Dr. Ann Della Maggiore.
In order to completely remove mass lesions, a surgeon needs a clear view of the large bowel’s anatomy. But this can be a challenging organ to image, especially as it passes through the bony pelvis, which limits an ultrasound’s penetration. And standard X-rays, don’t differentiate soft tissue structures with precision. Standard computed tomography (CT) isn’t commonly recommended for imaging assessment of the large bowel, because if the bowel isn’t evaluated while empty, the presence of fecal material can seriously limit the ability to identify and accurately describe mass lesions. Conversely, an empty bowel also produces limitations.
Colonoscopy is currently considered the gold standard for imaging lesions of the large bowel in dogs, because it provides an excellent view of the interior. But this technique doesn’t provide detailed information about the disease extent within the bowel’s wall or possible disease in nearby lymph nodes. CT pneumocolonography could be the solution. This technique is already used in the human medial field, and has proven to be safe, accurate, noninvasive and quick. It also supplies doctors with important data that colonoscopy alone cannot. This research is funded through the CCAH.
Researchers are currently recruiting dogs for this ongoing study — both those with mass lesions, as well as some without any known or palpable masses; for example, they may have inflammatory large bowel disease.
- TOP -

Study sheds light on home-cooked diets for dogs
A study funded by the CCAH evaluating the nutritional completeness of publicly available recipes for home-cooked diets for dogs drew major attention from veterinarians, dog owners and media outlets across the country.
Dr. Jonathan Stockman and Dr. Jennifer Larsen analyzed 200 dog food recipes in the largest-ever evaluation of the nutritional quality of home-prepared diets.
Published in June 2013 in the Journal of the American Veterinary Medical Association, the nutrition study looked at 200 recipes from 34 different sources, including websites, pet care books and veterinary textbooks, testing each meal to see if it met the basic dietary requirements for healthy adult dogs. Alarmingly, the vast majority of the recipes proved nutritionally deficient, which can lead to significant health problems.
“Ninety-five percent of the 200 diets we tested were deficient in at least one nutrient, and at least 84 percent were deficient in more than one nutrient,” explains Dr. Jennifer Larsen, assistant professor of clinical nutrition and one of the authors of the study. Among the nutrients found lacking were vitamin E, choline, and trace minerals such as zinc, copper and calcium.
The study was the largest-ever evaluation of the nutritional quality of home-prepared dog diets, which are sometimes favored by owners who prefer to prepare their dogs’ food themselves from fresh ingredients or who need to feed their animals a specialized diet due to diagnosed health issues. Larsen says that home-cooked diets are still a great option for many owners and their animals. But she recommends that owners avoid general recipes from books and the Internet. Rather, they should enlist the help of a board-certified veterinary nutritionist who can formulate a customized recipe that addresses all of their animal’s needs.
- TOP -

Keeping your pet safe in the Great Outdoors
Each year as the weather turns warm, not only do we enjoy the Great Outdoors, but so do many of our pets. However, there are hidden risks to our pets when they venture outside, even if it’s only in the back yard. Take precautions and be aware of lurking dangers that can sicken or injure our animal companions. Here are some tips for keeping your pet safe during the warm weather.
Tick and flea prevention is one of the most important things that can be done if your animal spends time outdoors.
Avoiding heatstroke
Increased outdoor temperature is a contributing factor to heatstroke, but it is an avoidable condition. An animal develops heatstroke when its body temperature rises to a dangerous point (often, over 106 degrees Fahrenheit) that will damage cell health and normal functions. Heatstroke often occurs during the first warm spell of spring, when a pet is not used to activity in warmer temperatures. Dogs at greater risk are those that are older, overweight and brachycephalic. Also at risk are pets left unattended in a parked car, which can reach dangerously high temperatures very quickly on a warm day.
“The best way to avoid heatstroke is to slowly reintroduce activity to your pet, while ensuring it has breaks for drinking plenty of water or cooling off in a pool or safe body of water,” says Dr. Karl Jandrey, an assistant clinical professor in the Small Animal Emergency and Intensive Care Service. If you suspect your pet is overheated — with signs of weakness, increased respiratory effort or rate, excessive “panting” (or not panting at all) or even vomiting — stop the activity. Cool your pet by soaking its coat down to the skin and then see a veterinarian as soon as possible. Drive with the air conditioning on, or if your pet is secured and away from the windows, have the windows down to encourage evaporative cooling. Always know the location of the closest emergency clinic, even when traveling.
Protecting against rattlesnake bites
Some dogs love to hike with their owners, especially as the weather warms. The risk of rattlesnake bites is most common between April and October. Here are some tips to help avoid rattlesnake bites:
- Keep away from areas with tall grass, rocks or wood piles
- Stay on trails and have your dog on a leash
- Use a walking stick to rustle brushes along the trail to alert snakes of your presence.
- If your dog is bitten, get to the nearest veterinarian quickly.
Preventing Infectious Diseases
Infections from fleas, mosquitoes and ticks: Cats and dogs that go outdoors are susceptible to infections transmitted by fleas, mosquitoes and ticks. Even though your pet may not leave the yard or have direct exposure to other animals, it’s still at risk for infection.
The most common disease transmitted by mosquitoes is heartworm disease. Since there are mosquitoes living year- round in many locations, the use of heartworm preventatives is an effective way to protect against this disease. In California, dogs are more likely to develop tick-borne diseases than cats, which include a febrile illness known as granulocytic anaplasmosis, and, in some parts of California (primarily Humboldt County), Lyme disease. Bartonella is a bacteria transmitted by fleas and possibly ticks (which manifests as cat scratch disease in people). It can cause heart problems in dogs, though most cats infected with Bartonella do not get sick at all. A variety of products is available to protect against ticks. Make sure to follow the manufacturer’s instructions, or the products will not be effective. “Cats are susceptible to toxicity from many tick products (permethrin and amitraz), so sometimes cats can get sick if they live with a dog using these products. If you have cats, make sure you use a product that is safe for cats, such as flumethrin or fipronil,” says Dr. Jane Sykes serves as director of the Small Animal Clinic in the veterinary hospital.
Check your pet for ticks after outdoor activities and remove any ticks promptly to help prevent the spread of tick-borne infectious diseases. Do not use bare hands when removing ticks — use a special device (or curved forceps). With the forceps, grasp the tick as close to the skin’s surface as possible. Pull upwards with steady, even pressure and make sure mouth-parts do not break off and remain in the skin. If that happens, disinfect the area and watch carefully for the possibility of infection. If you see signs of swelling or redness, your pet should be checked by a veterinarian.
Feline infectious diseases: Cats who spend time outdoors are at risk for a number of infectious diseases. The most common one is an abscess that occurs from an injury received during a fight with another cat. Cats who fight are also at risk for acquiring two viral infections: feline leukemia virus and feline immunodeficiency virus. These viruses can gradually impair a cat’s immune system. The end result, often several years later, may be cancer or other infectious diseases. Feline viral upper respiratory disease and feline panleukopenia virus are also transmitted between cats.
Leptospirosis: This disease is seen most often in dogs who are outdoors, but more often during times of warm and wet weather. Leptospires are bacteria that can cause fever and kidney failure in dogs. Dr. Sykes advises, “Good vaccines are available for the prevention of leptospirosis and are recommended for dogs who spend a lot of time outdoors.”
Other infectious diseases: Kennel cough is a respiratory illness contracted when cats or dogs are housed in close quarters. “If you are planning to travel and leave your pet at a boarding kennel, consult with your veterinarian and care provider for the proper vaccination requirements,” Dr. Sykes recommends. It is also important to allow time for adequate immune response.
- TOP -
Beware: pets and toxic plants
A surprisingly large number of common garden and household plants are toxic to pets, and reactions to toxicity range from mild to life-threatening. Pets, like young children, explore the world with their senses, and they are therefore vulnerable to accidental poisoning. Many of these plants make wonderful additions to the garden, but it's important to know which plants are toxic. Avoid planting these where pets (or children) will have frequent unsupervised access to the plants.
These 12 plants below are responsible for the majority of calls to our veterinary hospital about possible plant poisoning. The list was compiled by Director of Pharmacy Dr. Valerie Wiebe. The toxicity of the plants below varies according to the species of animal exposed (cat, dog, bird, etc.), the amount of the plant that was ingested, and the specific variety or species of the plant.
If you suspect your pet has ingested any of these plants, call your veterinarian immediately. Do not wait to see if symptoms appear, because in some cases of poisoning, by the time symptoms appear it's too late to save the animal.

Lilies (Lilium, all spp.): Ingesting any part of the plant can cause complete kidney failure in 36-72 hours. First symptoms appear in a few hours and may include appetite suppression, lethargy, vomiting. Cats are especially sensitive to lily poisoning, so be very careful to keep your cats away from liliies of any kind, including the Amaryllis, Easter lilies, and Stargazer lilies so often found in homes around the holidays.

Lily of the Valley (Convallaria majalis): Ingesting any part of the plant can cause cardiac dysrhythmias, vomiting, diarrhea, confusion, weakness, and even death. (Photo courtesy of freebigpictures.com web site).

Anemone (Anenome and Pulsatilla, family Ranunculaceae): Irritating to the mucus membranes, and can cause blisters, hemorrhagic gastritis, shock, convulsions, and death. (Photo is Japanese Anemone).

Aloe Vera (family Liliaceae): Vomiting, depression, diarrhea, anorexia, tremors, change in urine color.

Amaryllis (family Amaryllidaceaea, incl. Hippeastrum spp.) All species, including Belladonna Lily, are toxic, and especially dangerous to cats. The bulbs are the toxic part of the plant. The "Amaryllis" commonly seen during the December holidays are Hippeastrum species. Symptoms include vomiting, depression, diarrhea, abdominal pain, hyper-salivation, anorexia, tremors. (Photo courtesy of Ellen Zagory, UC Davis Arboretum).

Asparagus Fern (family Liliaceae): Allergic dermatitis, gastric upset, vomiting, diarrhea.

Daffodil (Narcissus): Vomiting, diarrhea. Large ingestions cause convulsions, low blood pressure, tremors, cardiac arrhythmias.

Philodendrons: Irritation, intense burning and irritation of the mouth, lips, tongue, excessive drooling, vomiting, difficulty swallowing.

Jade Plants (Crassula argentea): Vomiting, depressions, ataxia, slow heart rate.

Chrysanthemums: Vomiting, diarrhea, hyper salivation, incoordination, dermatitis.

Cyclamen (Cyclamen persicum): The tubers or rhizomes contain the toxic glycoside cyclanin, a terpenoid saponin. Ingestion can cause excess salivation, vomiting, diarrhea, heart rhythm abnormalities, seizures, or even death in rare cases.

Cycads (including Sago palm; cardboard palm; etc.): The "Sago palm" is a cycad, not a true palm, and all parts of the plant are poisonous. Symptoms include vomiting, lethargy, melena (black "tarry" feces), icterus (jaundice), increased thirst, hemorrhagic gastritis, bruising, coagulopathy, liver failure, and death. A northern California police dog, a patient at one of our Companion Animal Memorial Fund donor clinics, died in November 2011 after ingesting parts of this plant.
Common plants that are highly toxic but only rarely ingested by pets include:
- Angel's Trumpet (Brugmansia spp.)
- Castor bean (Ricinus communis)
- Daphne (Daphne spp.)
- Deathcamas & Meadow Deathcamas (Zigadenus venenosus)
- English yew (Taxus baccata)
- Foxglove (Digitalis purpurea)
- Jimson weed or Devil's Trumpet (many common names) (Datura spp.)
- Nicotiana/Tobacco plants (all spp.)
- Oleander (Nerium Oleander)
- Poison hemlock (Conium maculatum)
- Pokeweed (Phytilacca americana)
- Tree tobacco (Nicotiana glauca)
- Western water hemlock (Cicuta douglasii)
- Yew (Taxus cuspidata)
UCD Toxic Plant Garden Information
On the School of Veterinary Medicine campus, visitors can explore the Toxic Plant Garden (north of Vet Med 3A and south of Tupper Hall), which includes many plants commonly grown in Northern California known to be toxic to pets.
- TOP -

What is the West Nile virus?
The West Nile virus is a strain of encephalitis disease, genetically similar to St. Louis encephalitis, that can affect the central nervous system. WN virus causes a swelling of the brain that, though treatable, can be fatal in a small portion of infected people and animals. The virus can be carried by birds and transmitted by mosquitoes that feed on an infected bird and then feed on a human or animal.
Among wild birds, Corvids such as crows, scrub jays and magpies are particularly susceptible. Indeed, WN virus has had a significant impact on these and other bird species. Pet birds are probably at greater risk to WN virus than dogs or cats. Owners of pet birds should refer to the CDC website table of bird deaths from WN virus between 1999 and 2007. Pet species are usually classified as exotic in this table. (http://www.cdc.gov/ncidod/dvbid/westnile/)
Can small companion animals such as birds, cats and dogs contract WN virus?
Dogs and cats are susceptible to infection, but considerably more resistant to disease than horses, humans, and some species of birds. Very young and very old cats and dogs, and animals that are immunocompromised for some other reason, are the most likely to show signs of illness. Signs of a possible infection include weakness, fever and muscle spasms, although blood tests are needed to confirm a diagnosis. Treatment is consistent with standard veterinary practices for viral infections, and recovery is likely. If you suspect that your animal may be infected, seek the advice of your regular veterinarian.
How likely is it that my cat or dog will catch WN virus?
It is very unlikely for healthy dogs or cats to become ill with this virus. Pet owners should do the same things that they should do to protect themselves and family members: eliminate mosquito habitat and avoid mosquito exposure. Private veterinarians may also be consulted for recommendations on safe, effective mosquito repellents that may be used on pets. DEET-containing products are not approved for pets and should not be used. It is very important not to use human insect repellent on your animal as it may cause poisoning.
Can I contract the virus from my infected animal?
West Nile virus infection has been confirmed in some domestic animals, including pet birds, dogs and cats. However, there is no evidence that a person can get the virus from handling any animal, including live or dead infected birds. Furthermore, there is no evidence that West Nile virus can be transmitted to humans through consuming infected birds or animals.
There is no evidence that a person can get WN virus from handling live or dead infected birds. However, one should always use caution when handling dead birds. Persons should avoid bare-handed contact when handling any dead animals, and use gloves or double plastic bags to place the bird carcass in a garbage bag or contact their local health department for guidance.
Can the virus be transmitted from animal to animal?
It is possible that dogs and cats could become infected by eating dead infected animals such as birds, but this is undocumented. Veterinarians should take normal infection control precautions when caring for an animal suspected to have this or any viral infection.
How common is WN virus in California?
For information on WN virus in California please visit the California Vectorbourne Disease Surveillance Center's website http://westnile.ca.gov/. This site contains the most current information on the spread of WN virus in California.
What can I do to protect myself as well as my companion animals?
WN virus is transmitted by infectious mosquitoes. Dogs or cats could be exposed to the virus in the same way humans become infected. To protect your self as well as your animals these precautions are recommended:
- Make sure that doors and windows have tight-fitting screens. Repair or replace all screens that have tears or holes.
- Eliminate mosquito breeding sites from around your home (standing water).
- Don't go outside in the early evening or at dawn.
- If you are outdoors during those times, wear long-sleeved shirts and long pants. But bear in mind that mosquitoes can bite through thin cloth.
- Consider using insect repellent (the CDC recommends using one with permethrin or DEET) on your skin and clothing, particularly if you live in a wet, low-lying area where mosquitoes might breed. But use insect sprays sparingly and cautiously. (This means never spraying repellents on children under the age of three or on the hands of children who might put them in their mouths.) DEET-containing products are not approved for pets and should not be used. It is very important not to use human insect repellent on your animal as it may cause poisoning.
- Dispose of any unused outside water containers and drill holes in the bottom of containers that are left outdoors. Turn over plastic wading pools or wheelbarrows when not in use, and do not allow water to stagnate in birdbaths.
- Clean clogged roof gutters regularly.
- Ventilate ornamental pools or stock them with fish.
- Clean and chlorinate swimming pools that are not in use.
- If you have livestock, thoroughly clean their troughs every month.
- Don't rely on ultrasonic mosquito-repelling machines or vitamin B to ward off bites.
- TOP -
